“We just need help.”
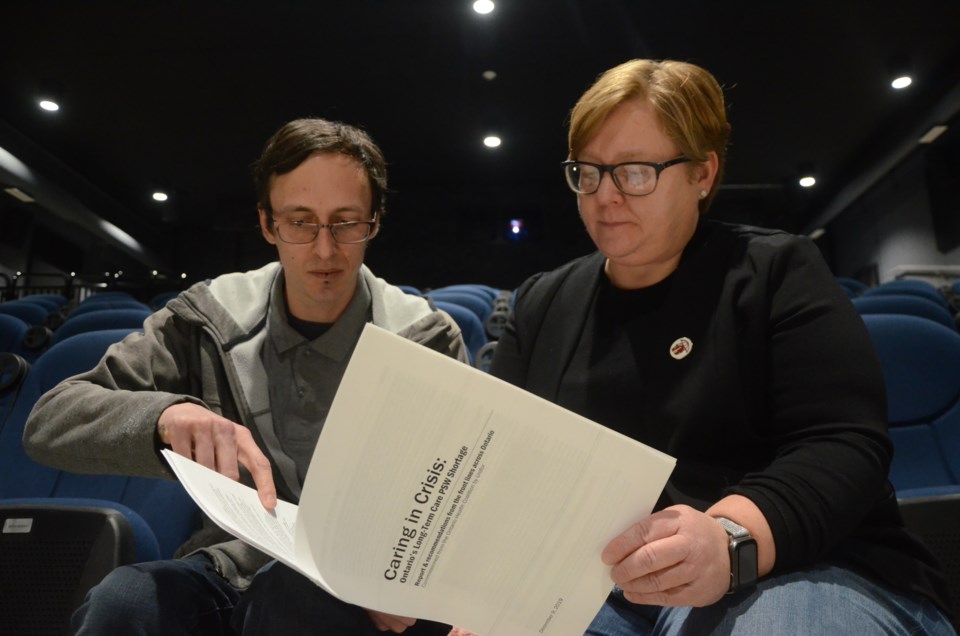
Those were words uttered by personal support worker Shawn Mathe, the member at large for the nursing care sector, Local 598, Unifor and the unit chair for Finlandia Village. He was speaking at the launch of a new report, “Caring in Crisis: Ontario’s Long-Term Care PSW Shortage,” written by the Ontario Health Coalition and commissioned by Unifor.
Mathe said there's an easy solution to address the shortage of PSWs across the province. PSWs need to be given the time they need to properly care for residents, and that decision rests with the provincial government.
“It's that simple,” Mathe said. “More time is all we need. We all take it for granted, but in this job, we need that time to provide the quality level of care we are expected to provide.
“It would be nice to have a staffing ratio of one PSW to four residents, or even one to five, but this one PSW to 13 or 15 residents is pushing us to the brink. There's going to be a breaking point, and it's going to be very sad to see that when it happens.
PSWs are subject to every type of abuse — physical, verbal, sexual — but are expected to put on a smile every day, Mathe said.
“Caring in Crisis” examines the PSW shortage in Ontario’s long-term care homes, and is based on the input and feedback from round-table meetings held across the province last year. Those meetings included home operators and administrators, PSWs, union representatives, family councils, seniors, college staff who develop/co-ordinate PSW courses, local health coalitions and other long-term care advocates.
In Ontario, there are about 80,000 long-term care residents. However, in every town, in virtually every long-term care home, on virtually every shift, long-term care homes are working short staffed, said the report.
Long-term care homes have reported they are working with shortages of one to two PSWs on almost all shifts, which means they can be short five to 10 PSWs in every 24-hour period. Some homes are short 20 to 50 PSWs, said the report.
Poor compensation, injuries and violence and impossible workloads are a few of the reasons cited for PSWs leaving the field, where turnover is very high and “burnout” is rampant.
Andy Savela, director of health care for Unifor, said they aren't just tossing around the term crisis.
“We aren't using that word lightly,” Savela said. “The situation is shameful, and our senior citizens are suffering. That's what we're really trying to highlight.”
PSWs are some of the hardest-working people in the province, but they often go home after their shift feeling disheartened because they feel they could have done more if they had the time, Savela said.
Compounding the shortage is the increasing complexity of care needs among long-term care residents, said the report. Residents are medically complex and frail, but care is being provided in environments not designed for such care and staffed with insufficient numbers of nurses and PSWs.
Government data reveals 81 per cent of long-term care residents have some form of cognitive impairment, with nearly one-third displaying severe cognitive impairment. As many as 86 per cent of individuals diagnosed with dementia will act aggressively as the disease progresses, and almost half of all residents in long-term care display aggressive behaviours.
To help solve the crisis, there needs to be an increase in the number of PSWs, but there are a number of barriers that stop people from taking courses. Courses cost $5,000 or more and child care costs can double that, making those courses unaffordable.
Furthermore, many PSW jobs are part time, but staff would work full-time hours, which means they aren't getting the benefits their full-time counterparts are receiving.
“I'm not sure how to make our job look amazing to others,” Mathe said. “I get to make people smile every day, or I might be that little ray of sunshine in an otherwise gloomy day for a resident, and that's why I go to work, and it makes me feel awesome.”
The report listed nine recommendations to address the PSW crisis:
- Provide enhanced funding to improve wages and working conditions for PSWs. Compensation must be competitive to attract staff to long-term care. Funding should be tied to increasing the number of full-time positions, reducing precarious work and improving wages and benefits.
- Levels of care in Ontario's long-term care homes must be improved, and this improvement must be mandatory and enforceable. Increased funding must go to improving care. The Ontario government must institute a regulated minimum care standard of an average of four hours of daily hands-on direct nursing and personal support per resident to provide care and protect from harm.
- A provincial human resource recruitment and retention plan must be developed with clear, publicly reported timelines and targets, and accountability for meeting these targets in order o implement the minimum care standard.
- Long-term care homes must be resourced with trained staff able to deal with the increasing responsive behaviours in the homes. Homes should have in-house Behavioural Support Ontario teams in addition to the four-hour minimum care standard.
- Provincial standards for PSW courses muse be set to ensure that students are prepared for the real work environment. Provide resources and leadership to create partnerships between college and PSW programs and long-term care homes, apprenticeships, paid co-op placements in long-term care and other real-world training and work experience as part of all PSW courses.
- Tuition costs muse be reduced; access to grants, daycare and other subsidies to support students must be provided.
- Staffing shortages must be reported to the Ministry of Health and posed in each home.
- A publicity campaign to share a positive image of persona support work must be developed to increase retention and attract students to the sector.
- Capacity in our public hospitals must be restored, including psychogeriatric and complex continuity care beds. The offloading of patients whose care needs are too complex to be appropriate for long-term care must be stopped.