Six years ago, Alicia Reid began having mysterious attacks that caused severe upper abdominal pain and what she describes as “uncontrollable attacks of vomiting.”
Subjected to a battery of diagnostic tests, the 24-year-old's doctors still didn't really know what was wrong with her.
“It was at this time that morphine was suggested as an at-home treatment in order to prevent additional unpleasant and unproductive visits to the ER,” Reid said.
Although the morphine was supposed to be short-term solution, three and a half years later, she was still on the drug. Her dosage started off small, but by last fall, it had quadrupled.
“My body had become fully dependent on the morphine, and my life put on hold because of it,” she said.
“I was constantly timing my outings with friends, when I could even make it out, always wondering if my prescription would last the week, then hounding the doctor's office when I knew it wouldn't.”
Four months ago, after being referred by her family physician, Reid visited a downtown Sudbury pilot program addictions clinic run by Health Sciences North, known as a Rapid Access Addiction Medicine (RAAM) clinic.
After letting the morphine leave her system — those 48 hours were “the absolute worst,” she said — Reid was put on suboxone, a less harmful type of opiate.
“My life has done a complete 180 since being on this suboxone,” Reid said, adding she feels “more alert, more myself” and can now consider going back to work and attending post-secondary education.
An emotional Reid shared her story Jan. 16 as the North East Local Health Integration Network released a strategy to deal with huge increase in opioid use and opioid addiction that has swept across North America, including Northern Ontario, which has one of the highest overdose rates in Ontario.
She was given a standing ovation by those at the press conference, which included many representatives of health-care organizations in the region, as well as Sudbury MPP Glenn Thibeault.
The strategy was developed by the North East LHIN's mental health and addictions advisory council, made up of service providers in the mental health field and those with lived experience.
The North East LHIN's base funding has been increased by $1.6 million to implement the opioid strategy.
Much of the new funding will go to expand the number of RAAM clinics in the north east region, such as the one where Reid received treatment. The clinics provide an addictions pathway between the clinic and different places where the client is likely to seek care.
That includes emergency departments, primary care providers, mental health and addictions agencies and withdrawal management programs.
Besides the Sudbury RAAM clinic, which opened just over two years ago, there will also be similar clinics in the North Bay, Sault Ste. Marie and Cochrane, as well as James Bay and Hudson Bay coastal communities (exactly where has yet to be determined).
Each of these RAAM clinics will serve people in their region through the use of the Ontario Telemedicine Network.
The new funding will also enhance and expand Community Based Withdrawal Management programs, allowing participants to continue to live at home while receiving treatment.
“We're really pleased to be able to see the injection of funding to be able to support the Opioid Strategy,” said Kate Fyfe, interim CEO of the North East LHIN.
“I think what was most exciting for me in the investment was the ability to provide a hub and spoke approach where we will be able to see RAAM clinics established across the Northeast, not just in the major urban areas, but be able to reach out to the remote communities to provide support.”
These clinics provide treatment not only to opioid addicts, but also those who abuse alcohol and other types of drugs, said Dr. Mike Franklyn, lead RAAM physician for Sudbury and the North East LHIN.
As for opioids, Northern Ontario is one of the worst places in the world for opioid prescribing and overdose deaths, he said.
He urges fellow physicians not to just cut patients off opioids, and make sure they get proper addictions treatment. Otherwise they could start purchasing street-level drugs.
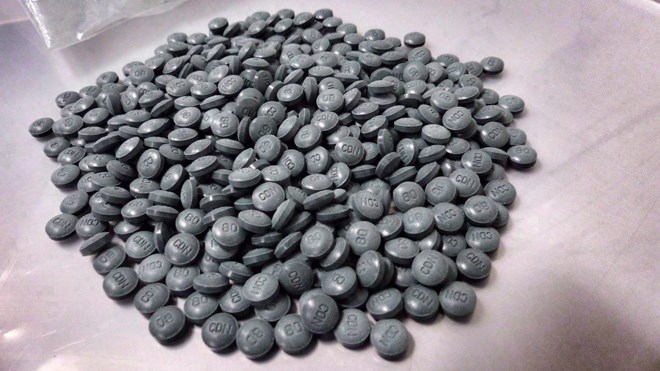
“I'm scared poopless of what's coming out there on the street,” he said. “It's never been a worse time to use the street opiate because of contamination with fentanyl and carfentanil.
“In the last two weeks of December, I lost two patients, both young mothers, one of one and one of three, to opiate overdoses. That's not atypical. That's going to get worse before it gets better. So there's an absolute need for this.”
If anyone reading this article is interested in treatment at the local RAAM clinic, phone Health Sciences North at 705-523-7100 for more information. Self-referrals are encouraged.