By Micheal Erskine
Manitoulin Expositor
MANITOULIN—It was just this past summer that Manitoulin found itself touted in the media as having the dubious distinction of having the highest number of opiod-related deaths per capita in the world, but more recent statistics contained in a November 2016 research report “Opiod Use and Related Adverse Events in Ontario” have relegated Manitoulin to 15th in that category.
The report, published by The Ontario Drug Policy Research Network, are according to the report, “a province-wide network of researchers who provide timely, high quality, drug policy relevant research to decision makers.”
“It is very hard to get up to date numbers,” noted Brenda Stankiewicz, a public health nurse with the Sudbury District Health Unit (SDHU). “We are usually about two years behind.”
The recent report, which covers opioid-related deaths over a five-year period between 2009 and 2013 (the most recent year for which statistics are available), averages yearly opioid-related deaths during this period per 10,000 population (using population estimates from Statistics Canada). The data on cause of deaths was obtained from the Office of the Chief Coroner of Ontario’s mortality data.
The report makes a strong attempt to offset the skewing that can come from extremely small datasets in some districts by presenting an annualized rate of opioid-related deaths over the five-year period between 2009 and 2013.
Asked to comment on the previous declaration that Manitoulin had the highest rates in the world, Ms. Stankiewicz suggested that might have been an extrapolated assumption—with some basis. When it came to prescribing opioids and opioid-related deaths, “Ontario had the highest rates in the country, Canada had the highest rates in the world,” she noted. It is a simple step from there to extrapolate that if Manitoulin had the highest rates in Ontario, it would hold the record for the world. “We don’t really have the information,” she noted.
Interesting comparisons note that Sudbury had 108 opioid-related deaths with a population of approximately 106,000. Sudbury ranks 27th in the number of opioid-related deaths per 10,000 population in Ontario. There were 49 counties and 14 Local Health Integrated Networks included in the study.
As with any scientific study, making the leap to direct conclusions in one particular area can be very complicated. With a population of approximately 13,000, Manitoulin registered less than five opioid-related deaths in 2013 and six over the range of 2009-2013.
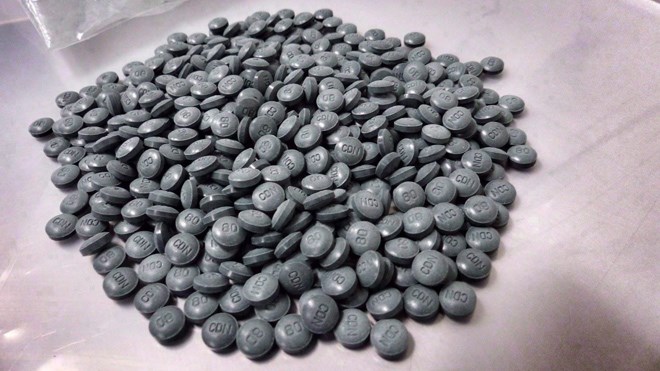
Another facet of the study that makes interpreting the data a bit challenging is the definition of “opioid.” While to the general public this would trigger a direct co-relation to drug abuse and the abuse of prescription drugs, that is not what the data is actually indicating. First off, the definition is actually quite broad. The code table for opioid-related hospital hospital admissions and emergency department visits includes: poisoning by opium, by heroin, other opioids, methadone, synthetic narcotics and “other and unspecified narcotics.”
A key challenge for determining opioid-related deaths lies in the data coming from the coroner’s office and the way causes of death have been assigned.
Often the actual cause of death may have been determined to have come about due to some other underlying cause, even though an opioid overdose may have been a contributing factor.
Nonetheless, Northern Ontario, both east and west, tend to have high rates of opioid use and abuse and the current introduction of new and more powerful opioids is setting off alarm bells in jurisdictions across Canada.
The report itself is a reaction to those concerns, noting: “the rising prevalence of abuse, misuse and addiction related to opioids has driven concerns regarding accidental opioid overdoses that may lead to hospitalizations for toxicity, and sometimes death. Indeed, in an analysis of opioid-related deaths abstracted from the Office of the Chief Coroner of Ontario, we found that rates of opioid overdose deaths increased 242 percent between 1991 and 2010. By 2010, there were 550 deaths related to opioid overdoses in Ontario, many of them in young people, representing a major impact on public health.”
The scale of the issue is in itself daunting. According to the report there were 660,674 opioid users in Ontario in 2015, 33,693 maintenance therapy users (methadone and suboxone etc.), 3,241 opioid related emergency department visits in 2014 and 638 opioid-related deaths in the province in 2013. Of those deaths, the vast majority fall in the two middle age cohorts, 25-44 at 283 to 45-64 at 279.
This isn’t an issue of youth—those in the know say that with age comes pain.
But when it comes to opioid-related hospital admissions in 2014, the numbers skew alarmingly. Although the number of opioid users in the under 25 category is less than a third of that of the 25-44 crew, and barely an eight of the 45-64 bunch, they have half the number (631 to 1,129 and 1,039) of opioid-related emergency department visits and (191 to 388 and 632) opioid-related hospital admissions.
On Manitoulin, there were less than five hospital admissions (ranking the Island 12th) and six emergency department visits (that place us eighth). In terms of opioid deaths, Manitoulin again had less than five in 2013 (for a rank of 15) and when averaged over five years the number stands at six (for a ranking of seventh).
There is a silver lining to the high number of Island residents undertaking replacement therapy in which the Island ranks second, noted Ms. Stankiewicz. “That to me is a good news story,” she said. “People are looking for help.”
The options available are expanding, with new treatments such as suboxone showing promise and the ready availability of the opioid antidote naloxone may help to reduce the number of deaths.
“There are important things to know when it comes to being with someone who is experiencing an overdose,” said Ms. Stankiewicz. “First call 911, call for help. Second, keep them breathing,” she said. This may well involve artificial resuscitation.
“Opioids slow down your brain, so your brain stops telling your body what to do,” she said. “So you stop breathing.” But opioids tend to be very short lived in that respect, so keeping someone breathing until they start again on their own can have a big impact.
"Third, administer naloxone and fourth, and this is very important, stay with the person until help arrives.”
Published by The Manitoulin Expositor. Reprinted with permission.